When patients are first diagnosed with pancreatic cancer, the cancer usually has spread to other organs. Because of these metastases, nearly all patients will succumb to their cancer within one year of diagnosis, but no drugs exist to prevent metastasis.
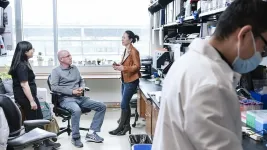
In an effort to find treatments, cancer researchers at Columbia--led by Anil K. Rustgi, MD, and Jason R. Pitarresi, PhD--investigated a hormone called PTHrP. Although PTHrP (parathyroid hormone-related protein) is often highly active in patients with pancreatic cancer, its role in metastasis was unclear.
Loss of PTHrP Dramatically Improves Survival in Mice
The researchers first manipulated the levels of PTHrP in mice with pancreatic cancer. Elimination of PTHrP from mice--with genetic engineering or with an antibody that targets the hormone--not only eliminated metastasis and enhanced overall survival, but also dramatically reduced the size of the initial tumors in the pancreas.
Even in mice with a highly aggressive form of pancreatic cancer, the increase in survival was dramatic, increasing from a median of 111 days to 192 days, with near complete elimination of metastases. The 73% increase in survival, the researchers say, is one of the largest observed in mice with this type of pancreatic cancer, which closely resembles human cancers.
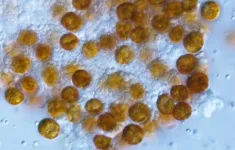
The striking results with mice led the researchers to test the anti-PTHrP antibodies in human pancreatic cancer cells. The results from these experiments were also encouraging: Among 3D organoids derived from pancreatic cancer patients under an IRB-approved protocol, anti-PTHrP antibodies greatly reduced growth and viability of the cells.
Two-Pronged Attack on Cell Growth and Metastasis
Targeting PTHrP attacks pancreatic cancer in two ways, the researchers say. It reduces the ability of the tumor cells to transition from an epithelial state to a mesenchymal state, which is necessary for the creation of new metastases. And targeting PTHrP also prevents the growth of primary and secondary tumors.
"We think these findings provide a strong rationale for further developing anti-PTHrP therapy towards clinical trials," says Rustgi, who adds that the antibody used in the study has the potential to be used in people and credits Richard Kremer, MD, PhD, of McGill University for developing the antibodies.
"We are hopeful that a drug targeting PTHrP could be used to treat most patients with pancreatic cancer," he says, "because the vast majority have tumors with high levels of PTHrP. There is the potential application to other cancers as well."
Potential with Other Cancers
The researchers originally began investigating PTHrP because its gene is often amplified when another nearby gene, KRAS, is amplified. KRAS has long been recognized as a cancer-promoting gene in pancreatic and other cancers.
For patients, that may mean anti-PTHrP therapies may have potential in other cancers that are known to harbor KRAS amplifications.
For researchers, the finding also suggests a wider search for cancer-causing genes is needed.
"We feel that PTHrP may have been previously overlooked as a mere passenger gene co-amplified with KRAS, but our study shows that PTHrP has its own tumor-promoting functions," Pitarresi says. "It suggests other so-called 'passenger' genes may have bigger roles in cancer than we initially thought and should be examined more closely." Rustgi notes "it might open up for combinatorial therapies of targeting the KRAS pathway with an antibody to PTHrP."
INFORMATION:
More Information
The research appears in Cancer Discovery in a paper titled "PTHrP drives pancreatic cancer growth and metastasis and reveals a new therapeutic vulnerability."
Anil K. Rustgi, MD, is interim executive vice president and dean of the Faculties of Health Sciences and Medicine at Columbia University and the director of the Herbert Irving Comprehensive Cancer Center at Columbia University Irving Medical Center/ NewYork-Presbyterian Hospital.
Jason R. Pitarresi, PhD, is a member of the Rustgi lab and a research associate in gastroenterology in the Department of Medicine at the University of Pennsylvania Perelman School of Medicine where Rustgi was before joining Columbia.
Other authors: Robert J. Norgard (Penn), Anna M. Chiarella (Columbia), Kensuke Suzuki (Columbia), Basil Bakir (Columbia), Varun Sahu (Columbia), Jinyang Li (Penn), Jun Zhao (University of Texas MD Anderson Cancer Center), Benoît Marchand (Columbia), Maximilian D. Wengyn (Penn), Antony Hsieh (Penn), Il-Kyu Kim (Penn), Amy Zhang (University of Toronto), Karine Sellin (McGill University), Vivian Lee (Penn), Shigetsugu Takano (Chiba University), Yoji Miyahara (Chiba University), Masayuki Ohtsuka (Chiba University), Anirban Maitra (MD Anderson Cancer Center), Faiyaz Notta (University of Toronto), Richard Kremer (McGill University), and Ben Z. Stanger (Penn).
This work was supported by the U.S. National Institutes of Health (grants F32CA221094, P30CA01369644, R01DK060694, and R01CA229803); an American Cancer Society Professorship (Rustgi); an American Gastroenterology Association's Bern Schwartz Research Scholar Award in Pancreatic Cancer; a Hopper-Belmont Foundation Inspiration Award; U.S. Department of Defense (grant W81XWH-15-1-0723); Canadian Institutes of Health Research (grant MOP142287); and an American Cancer Society-Fairfield County Comedy Against Cancer Postdoctoral Fellowship (PF-19-227- 01-CMS).
Richard Kremer is the inventor of the therapeutic monoclonal anti-PTHrP antibodies used in this study and authorized for use by Biochrom Pharma. RK is founder and president of Biochrom Pharma. All other authors declare no potential conflicts of interest.
Columbia University Irving Medical Center provides international leadership in basic, preclinical, and clinical research; medical and health sciences education; and patient care. The medical center trains future leaders and includes the dedicated work of many physicians, scientists, public health professionals, dentists, and nurses at the Vagelos College of Physicians and Surgeons, the Mailman School of Public Health, the College of Dental Medicine, the School of Nursing, the biomedical departments of the Graduate School of Arts and Sciences, and allied research centers and institutions. Columbia University Irving Medical Center is home to the largest medical research enterprise in New York City and State and one of the largest faculty medical practices in the Northeast. For more information, visit cuimc.columbia.edu or columbiadoctors.org.